Diagnosing the access problem: Canada can do more to ensure global access to vital diagnostic tools
Before patients can receive the right treatment, they need the right diagnosis. Despite their vital importance, access to diagnostic tools has never attracted as much attention as access to medicines. As with medicines, the 21st Century has seen major advances in diagnostic technologies. Unfortunately, affordability and accessibility haven’t kept pace, meaning even diagnostics well-suited for use in remote or low-resource environments are often unavailable where they are most needed.
One important diagnostic tool that remains widely inaccessible is the GeneXpert suite of tests, sold by diagnostics manufacturer Cepheid and its parent corporation Danaher. The best-known GeneXpert test is for diagnosing tuberculosis, but they also exist for other diseases, including HIV, COVID-19, Hepatitis C and mpox. The price of these tests unfortunately makes them unaffordable in many places where they would be most impactful.
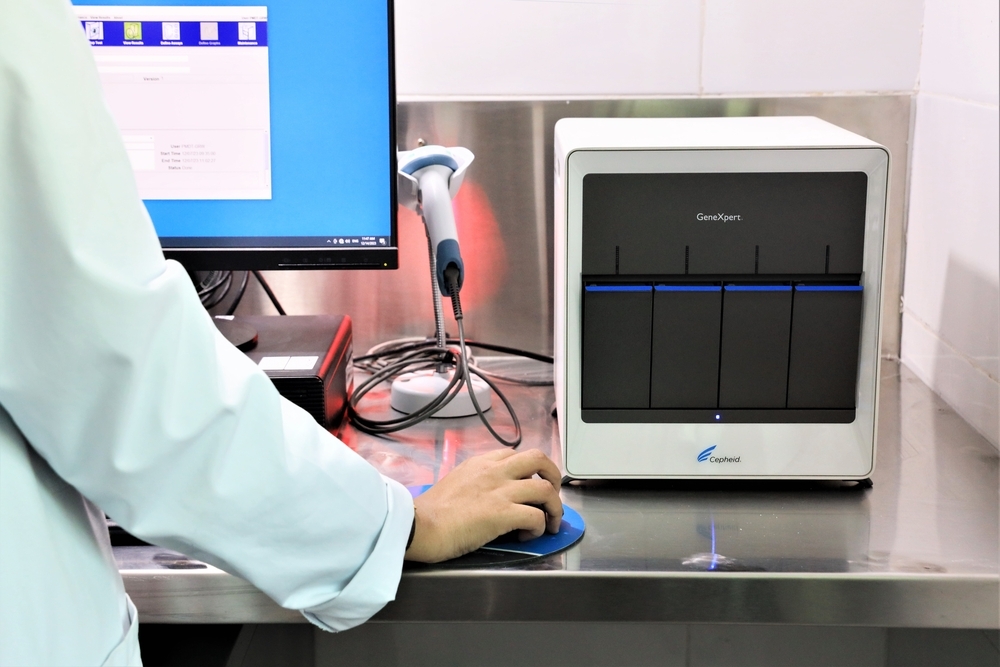
GeneXpert tests are priced between $8-20USD in lower-income countries, which yields up to 400 per cent profit margins (the price, and profit margin, is considerably higher in wealthy countries like Canada). An analysis published by Doctors Without Borders/Médecins Sans Frontières (MSF) shows the cost of manufacturing, plus a reasonable profit margin could be achieved at a price of $5. This is the impetus for the Time for $5 Campaign, in which over 200,000 supporters have called upon the companies behind GeneXpert to bring the price down to that level for low and middle-income countries (LMICs).
Canada can play an important role in securing this price reduction. Canada has long been a major funder of global health mechanisms like The Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), who drive large purchases of diagnostic tests. While needs still outweigh funding, Canada has shown leadership, notably during the 2022 Global Fund replenishment, when Canada stepped up to meet calls to increase its financial contributions by 30 per cent. Canada is not only a major donor to Global Fund, but currently holds a seat on its board; Canada can use this dual influence to prioritize ensuring diagnostics are affordable and accessible.
Cheaper diagnostics mean financial contributions like Canada’s have greater impact. More importantly, they mean more people getting diagnosed, allowing them to receive treatment more quickly. A price decrease can have considerable implications. In the fall of 2023, Cepheid and Danaher responded to the Time for $5 campaign by decreasing the price of a single GeneXpert test for tuberculosis from $10 to $8; this means dollars spent on this test go 20 per cent further. Lowering the price all the way to $5, and for all GeneXpert tests across all diseases, will make a real difference in how many tests can be procured, and people diagnosed. Danaher also committed to an annual third-party cost assessment of GeneXpert tests, but after nearly a year without updates, civil society is calling for this promised audit to be conducted in a timely, rigorous and transparent manner.

Although cost isn’t as great an access barrier in wealthy countries like Canada, tools permitting rapid diagnosis in remote regions, like the North, remain important. Of course, diagnosis is only the first step towards treatment and cure, and here profit motives again undermine public health; many drugs used in faster, safer, globally-recognized treatment regimens are not marketed in Canada because pharmaceutical companies do not see “the market” as big enough to be sufficiently lucrative.
Access issues are a symptom of underlying problems in how Canada invests in health, which must be diagnosed and treated. A crucial response is not only to invest more in diseases like TB, but to ensure the benefits of those investments flow to those who need them. Many innovations heavily rely on public funding for their development; Cepheid received at least US$250 million in public funds for the R&D behind GeneXpert. However, in Canada as elsewhere, the benefits from products developed with public money accrue primarily to private companies. GeneXpert shows a reasonable profit can be made while keeping prices affordable. To address future situations where manufacturers receive public investments to support their R&D but charge unaffordable prices to LMICs, Canada should take proactive measures in the Pandemic Agreement negotiations and at home to attach conditions to public health research funding to ensure that resulting products are both affordable and accessible to all. In turn, more affordable products will mean Canadian funding at home and abroad will stretch farther. Saving more lives will be a good return on Canadian investment.